Areas of Interest
Find your path to success at Green River College!
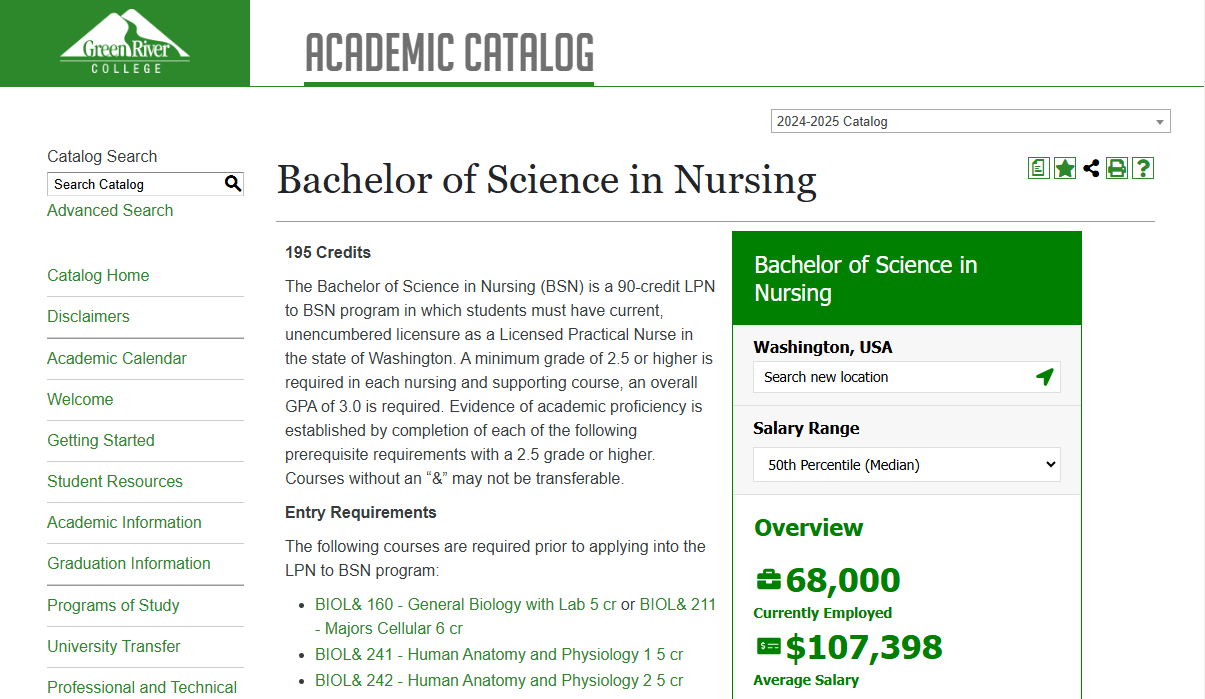
To help you navigate your college journey, GRC offers 7 academic and career pathways, opportunities to Study Abroad, and resources for those who are undecided. Whether you aim to enter the workforce immediately after graduation or pursue higher studies in your chosen field at a university, our pathways offer the flexibility and support required. With access to over 100 degrees, certificates, electives, and resources, you can tailor your educational experience to suit your unique goals and aspirations.
General Areas
Browse Catalog
Information for current and perspective students about Green River College's academic programs, programs of study, and more.

Paying for School
Paying for college is a challenge for most students, but we can help! We're confident you'll find Green River College provides a high quality education at an affordable rate.
Areas of Interest Pathways

Business & Entrepreneurship


Education, Law, & Social Sciences


High School, College Prep, & ELL


Fine Arts & Humanities


Healthcare & Wellness


Science, Technology, Engineering, & Mathematics (STEM)
 Are you intrigued by solving problems in the physical and natural world? The STEM
pathway will help you understand the world through observation and experimentation.
Whether you dream of discovering new medicines, creating cutting-edge software, or
addressing global warming, we'll prepare you for an exciting journey of scientific
exploration.
Are you intrigued by solving problems in the physical and natural world? The STEM
pathway will help you understand the world through observation and experimentation.
Whether you dream of discovering new medicines, creating cutting-edge software, or
addressing global warming, we'll prepare you for an exciting journey of scientific
exploration.
Skilled Trades, Industrial Technology, Aviation, and Natural Resources
 Do you see the value in hands-on skills that keep our world running smoothly? Green
River College’s Skilled Trades & Technical Training programs emphasize practical instruction,
problem-solving abilities, and creative thinking. Whether you aspire to work with
your hands as an automotive mechanic, welder, carpenter, machinist, or mechatronics
technician, launch a career in aviation as a pilot or air traffic controller, or protect
our natural resources as a forestry technician, you will be empowered with the skills
needed for a fulfilling career.
Do you see the value in hands-on skills that keep our world running smoothly? Green
River College’s Skilled Trades & Technical Training programs emphasize practical instruction,
problem-solving abilities, and creative thinking. Whether you aspire to work with
your hands as an automotive mechanic, welder, carpenter, machinist, or mechatronics
technician, launch a career in aviation as a pilot or air traffic controller, or protect
our natural resources as a forestry technician, you will be empowered with the skills
needed for a fulfilling career. Still Undecided?
There is a path for you. Let us help you get started.
Learn About Your Options at Green River